Understanding Glaucoma Surgery Costs in Australia
Glaucoma, a leading cause of irreversible blindness worldwide, poses significant health challenges for many individuals. For patients diagnosed with this condition, understanding the costs associated with glaucoma surgery in Australia is crucial when weighing their treatment options.
What is Glaucoma?
Glaucoma australia is a group of eye diseases characterized by damage to the optic nerve, often caused by elevated intraocular pressure (IOP). This pressure can result from an imbalance between the production and drainage of aqueous humor, the fluid within the eye. The optic nerve is crucial for transmitting visual information from the eye to the brain, and any damage to it can lead to significant vision impairment or even blindness if not managed properly.
The Basics of Glaucoma
The development of glaucoma is usually gradual, and many people are unaware they have it until significant damage has occurred. Regular eye examinations are essential for early detection, as vision loss from glaucoma is irreversible. The condition primarily affects peripheral vision initially, leading eventually to tunnel vision if left untreated. Symptoms may not appear until the disease has progressed, making it vital for individuals, especially those at higher risk, such as those with a family history of glaucoma or those over the age of 60, to have regular screenings. Early intervention can help manage the disease and preserve vision.
Types of Glaucoma
Open-Angle Glaucoma: The most common form, occurring when the drainage system for the eye becomes clogged over time. This type often progresses slowly and can go unnoticed for years.
Angle-Closure Glaucoma: A less common but more acute type, where the lens of the eye contacts the iris, blocking the drainage angle. This can cause sudden symptoms such as severe eye pain, headache, nausea, and vomiting, requiring immediate medical attention.
Normal-Tension Glaucoma: A type where optic nerve damage occurs even with normal eye pressure. The reasons for this type are not fully understood, but it may be related to reduced blood flow to the optic nerve.
Congenital Glaucoma: A rare form that develops in infants due to abnormal eye development. Early diagnosis and treatment are crucial to prevent permanent vision loss in affected children.
In addition to these primary types, there are also secondary glaucomas, which can develop as a result of other medical conditions or injuries to the eye. For instance, conditions such as diabetes or inflammation can contribute to the development of glaucoma, making it imperative for individuals with these conditions to monitor their eye health closely. Furthermore, lifestyle factors such as diet, exercise, and adherence to prescribed medications can play significant roles in managing intraocular pressure and overall eye health.

The Need for Glaucoma Surgery
While glaucoma can often be effectively managed with medication and lifestyle changes, surgery may be necessary for more advanced cases or when other treatments have failed. Understanding when surgery is warranted is crucial for patients dealing with this condition. Early detection and timely intervention can play a significant role in preserving vision and preventing the progression of this potentially debilitating disease.
Symptoms Leading to Surgery
Patients may experience several symptoms that can indicate the need for surgical intervention, including worsening peripheral vision, increased sensitivity to light, and halos around lights. As these symptoms progress, patients often find it increasingly difficult to perform everyday tasks, prompting the need for more aggressive treatment options. Additionally, some patients may report frequent headaches or eye pain, which can further signal the urgency for surgical evaluation. It is essential for patients to maintain open communication with their eye care professionals about any changes in their symptoms, as this can guide the decision-making process regarding surgery. Read more about identifying symptoms of glaucoma at https://health.ucdavis.edu/conditions/vision-eye-health/glaucoma
Risks of Not Undergoing Surgery
Delaying or avoiding surgery can lead to serious long-term consequences. Without intervention, individuals may face irreversible vision loss, which can significantly impact their quality of life. The risks include complete blindness and an increased dependency on others for daily activities. Moreover, the psychological toll of living with advanced glaucoma can lead to anxiety and depression, as patients grapple with the fear of losing their independence. It is vital for patients to weigh these risks against the potential benefits of surgery, which can not only stabilize their vision but also enhance their overall well-being and ability to engage in life fully.
Overview of Glaucoma Surgery Procedures
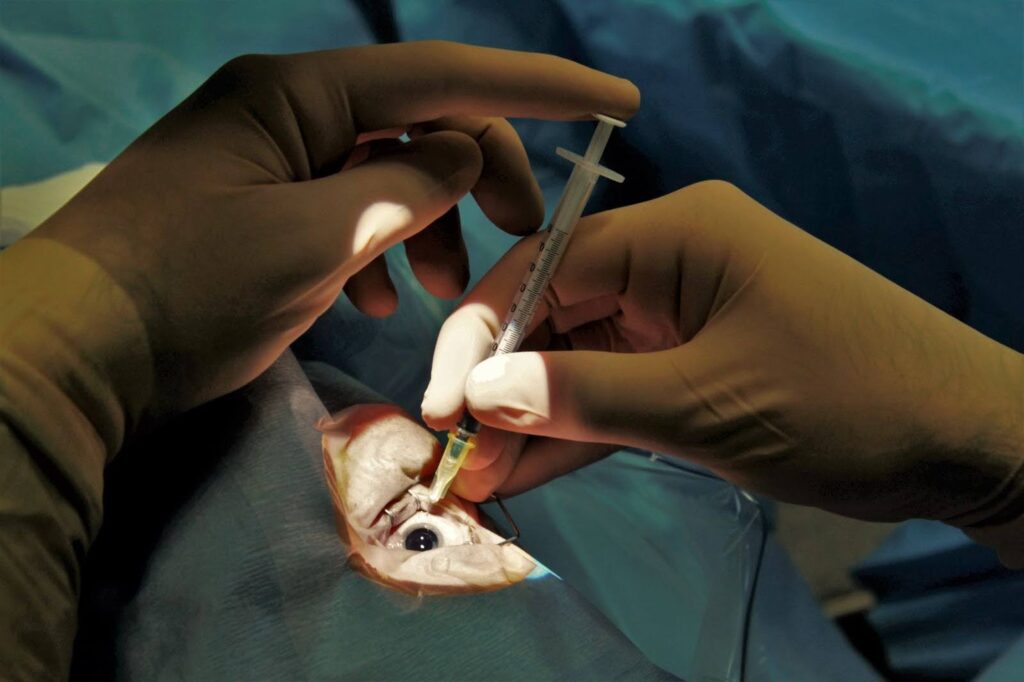
There are several surgical options available for treating glaucoma, each tailored to the specific needs of the patient. A comprehensive understanding of these procedures can help patients make informed decisions about their treatment.
Laser Surgery for Glaucoma
One of the least invasive options is laser surgery, which helps improve the outflow of fluid and reduce eye pressure. Procedures like Selective Laser Trabeculoplasty (SLT) are often performed in outpatient settings and can be effective in reducing IOP without significant recovery time. This technique utilizes a laser to target specific cells in the trabecular meshwork, enhancing the drainage of aqueous humor. Patients typically experience minimal discomfort during the procedure, and many return to their normal activities almost immediately. Additionally, SLT can be repeated if necessary, making it a flexible option for long-term management of glaucoma.
Trabeculectomy: A Common Glaucoma Surgery
Trabeculectomy is a surgical procedure that creates a new drainage pathway for the aqueous humor, thereby lowering eye pressure. While effective, it requires a longer recovery period and has risks, including infection and scarring. Post-operative care is crucial, as patients may need to attend follow-up appointments to monitor their eye pressure and the healing process. The success of trabeculectomy can vary, with some patients achieving significant pressure reduction while others may require additional treatments. Furthermore, advancements in surgical techniques and postoperative medications have improved outcomes, allowing for better management of potential complications. Understanding these nuances can empower patients to engage in discussions with their ophthalmologists about the best surgical options for their individual circumstances.
Breakdown of Glaucoma Surgery Costs
Understanding the financial aspect of glaucoma surgery is essential for patients and their families. Costs can vary widely based on various factors, including the type of procedure and hospital fees.
Pre-Surgery Costs
Prior to surgery, patients may incur costs related to initial consultations, diagnostic testing, and medication. Eye examinations can also add to out-of-pocket expenses. Patients should budget for these costs, as they may not be fully covered by insurance plans. In addition to these expenses, patients might also need to consider the costs of transportation to and from medical appointments, especially if they require frequent visits to specialists. This can add up significantly, particularly for those who live in rural areas where access to eye care facilities is limited.
Surgery Procedure Costs
The actual cost of surgery can depend on the type of surgical procedure performed. Laser surgeries are generally less expensive than more invasive techniques like trabeculectomy. Additionally, facility fees and the surgeon’s experience can contribute to overall costs. It’s also important to note that some patients may qualify for financial assistance programs or sliding scale fees based on their income, which can help mitigate the financial burden. Patients should actively communicate with their healthcare providers to explore all available options and ensure they understand the full scope of potential costs associated with their chosen procedure.
Post-Surgery Costs
Following surgery, patients may incur costs related to follow-up consultations, ongoing medication, and possible additional treatments. Regular monitoring is essential to ensure the ongoing effectiveness of the surgery, which can also contribute to long-term financial considerations. Furthermore, some patients may experience complications that necessitate further interventions or additional therapies, which can significantly increase overall expenses. Patients should also consider the potential need for lifestyle adjustments or assistive devices, such as specialized eyewear or home modifications, to accommodate any changes in vision post-surgery. These factors can further complicate the financial landscape surrounding glaucoma treatment and underscore the importance of thorough planning and communication with healthcare providers. To learn more about after surgery comforts and discomforts click here.
Factors Affecting Glaucoma Surgery Costs
Several factors can influence the overall cost of glaucoma surgery in Australia, making it important for patients to understand these elements before undergoing treatment.
Location and Hospital Fees
The geographical location of the hospital or clinic can affect surgical costs significantly. Urban centers often have higher fees compared to rural areas due to increased overheads and demand for services. Patients should consider these factors while choosing their treatment facilities. Additionally, the type of facility—whether it’s a public hospital, private hospital, or specialized eye clinic—can also lead to variations in costs. Public hospitals may offer lower fees, but waiting times can be longer, whereas private facilities might provide quicker access to surgery but at a premium price.
Surgeon’s Experience and Reputation
The experience and track record of the surgeon can also play a role in costs. Highly reputed surgeons may charge more for their expertise, while less experienced practitioners may offer lower fees. However, patients should weigh costs against potential outcomes and the surgeon’s skill in managing complex cases. It’s also worth noting that some surgeons may have affiliations with specific hospitals or clinics, which could influence the overall cost structure. Patients are encouraged to research their surgeon’s background, including patient reviews and success rates, to ensure they are making an informed decision.
Type of Surgery Performed
Finally, the specific kind of surgical procedure can greatly impact the final bill. Laser surgeries generally have lower associated costs compared to traditional surgical methods. Patients should discuss the pros and cons of various surgical options with their healthcare providers to choose the most suitable and cost-effective method. Furthermore, the complexity of the individual case can lead to additional costs, such as pre-operative assessments, post-operative care, and potential follow-up treatments. Understanding the full scope of these expenses is crucial for effective financial planning.
Moreover, patients should also consider the potential need for additional treatments or medications following surgery, which can add to the overall cost. Some patients may require ongoing monitoring or additional procedures to ensure optimal outcomes. It is advisable for patients to have a detailed discussion with their healthcare providers about the expected post-operative care and any associated costs to avoid unexpected financial burdens. This proactive approach can help patients better prepare for the financial aspects of their treatment journey.
Related : Symptoms and Treatment Options for Glaucoma: A Comprehensive Guide