Symptoms and Treatment Options for Glaucoma: A Comprehensive Guide
Glaucoma is a complex and often misunderstood eye condition that affects millions worldwide. Understanding its symptoms and various treatment options is crucial for early detection and management. This comprehensive guide will delve into the nature of glaucoma, how to recognize its symptoms, and the different diagnostic and treatment strategies available.
Understanding Glaucoma
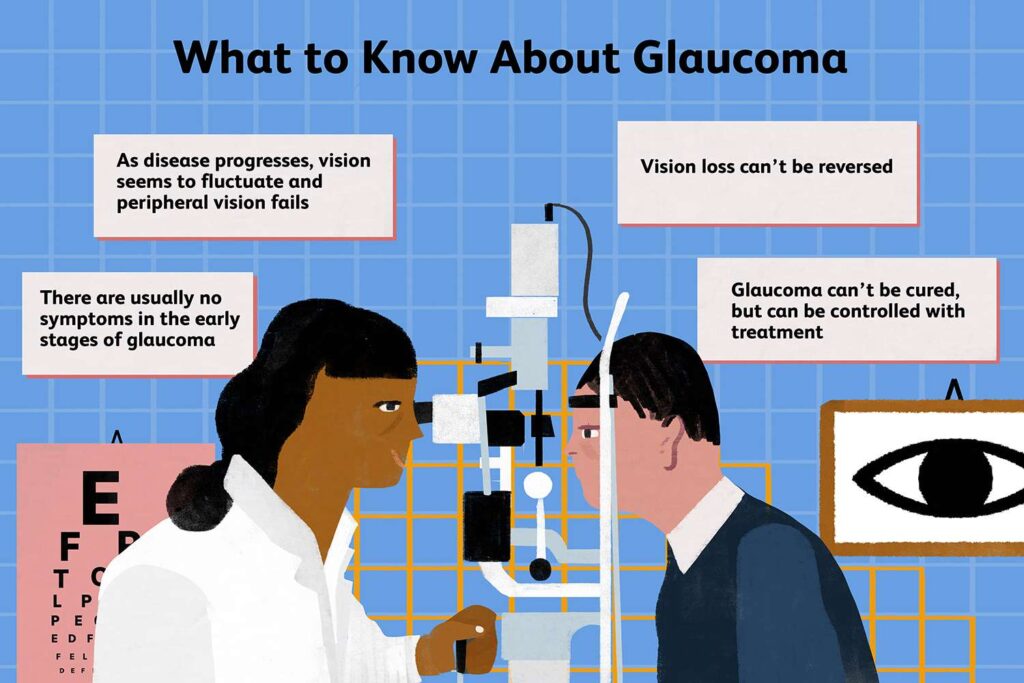
Eye glaucoma is a group of eye disorders that result in damage to the optic nerve, typically due to high intraocular pressure (IOP). Over time, this damage can lead to vision loss and even blindness. It is often referred to as the “silent thief of sight” because it may not exhibit symptoms until significant damage has occurred.
What is Glaucoma?
At its core, glaucoma involves the progressive degeneration of the optic nerve. The pressure buildup in the eye occurs when the fluid known as aqueous humor does not drain properly, either due to blockage or other mechanisms. Two main types of glaucoma exist: primary open-angle glaucoma, which is the most common, and angle-closure glaucoma, which can present as a medical emergency.
Primary open-angle glaucoma develops gradually and is often asymptomatic in the early stages. On the other hand, angle-closure glaucoma can occur suddenly, leading to severe symptoms such as intense eye pain, nausea, and blurred vision. Understanding these distinctions can be pivotal for timely diagnosis and treatment. In fact, regular eye check-ups are crucial, as they can help detect changes in eye pressure and optic nerve health before significant damage occurs.
Causes and Risk Factors of Glaucoma
While the exact causes of glaucoma remain uncertain, several risk factors have been identified. Age is a significant factor, as the likelihood of developing glaucoma increases with age, particularly after 60. Additionally, individuals with a family history of glaucoma are at a higher risk, indicating a potential genetic component.
High intraocular pressure
Thin corneas
Previous eye injuries or surgeries
Long-term use of corticosteroid medications
Certain medical conditions, like diabetes and high blood pressure
Being aware of these risk factors can empower individuals to seek regular eye examinations, especially those falling into high-risk categories. Furthermore, lifestyle choices can also play a role in managing eye health. For instance, maintaining a healthy diet rich in antioxidants, engaging in regular physical activity, and avoiding smoking can contribute positively to overall eye health. Some studies suggest that omega-3 fatty acids may even help in reducing the risk of developing glaucoma, highlighting the importance of nutrition in eye care.
In addition to lifestyle factors, advancements in medical technology have led to improved diagnostic techniques for glaucoma. Optical coherence tomography (OCT) allows for detailed imaging of the optic nerve and can detect early signs of damage that may not be visible through traditional examination methods. This technological progress underscores the importance of regular eye check-ups, as early detection remains the key to managing glaucoma effectively and preserving vision.
Recognizing the Symptoms of Glaucoma
Timely recognition of glaucoma symptoms is crucial for preventing irreversible damage. Many people may not notice symptoms until substantial vision loss has occurred, emphasizing the importance of regular eye check-ups. Glaucoma is often referred to as the “silent thief of sight,” as it can progress without any noticeable signs, making awareness and education about the condition vital for early intervention. Learn more about the term silent thief of sight and how it is related with glaucoma at https://ophthalmology.wustl.edu/glaucoma-awareness-detecting-and-managing-the-silent-thief-of-sight/
Early Warning Signs
In the early stages of primary open-angle glaucoma, there are usually no noticeable symptoms. Some individuals may, however, notice slight changes in their peripheral vision over time. Conversely, in cases of acute angle-closure glaucoma, symptoms can manifest quickly and include severe headaches, eye pain, nausea, and sudden disturbances in vision. These acute symptoms often prompt immediate medical attention, highlighting the need for individuals to be aware of their eye health and any sudden changes they experience.
Regular eye examinations, including measuring IOP and assessing the optic nerve, can detect early signs of glaucoma, ideally before significant damage has occurred. Eye care professionals may also utilize advanced imaging techniques, such as optical coherence tomography (OCT), to visualize the optic nerve and monitor any changes over time, providing a more comprehensive understanding of an individual’s eye health.
Progression of Symptoms
As the disease progresses, individuals may experience a gradual loss of peripheral vision, which can culminate in tunnel vision or complete blindness if left untreated. Symptoms can become more pronounced, impacting daily activities. This gradual decline can be particularly insidious, as many may not realize the extent of their vision loss until it significantly interferes with their quality of life.
Recognizing these changes is fundamental. For instance, individuals may have difficulty reading, driving, or engaging in activities that require visual acuity. The impact of glaucoma extends beyond just vision; it can affect mental health, leading to feelings of frustration, anxiety, and isolation. If you or someone you know is experiencing these symptoms, consulting an eye care professional promptly is essential. Early detection and management can help preserve vision and maintain a better quality of life, underscoring the importance of vigilance and proactive care in eye health.
Diagnostic Procedures for Glaucoma
Diagnosing glaucoma typically requires several diagnostic tests to evaluate the eye’s health thoroughly. These tests are essential in determining the presence and severity of the disease.
Eye Examination
A comprehensive eye examination includes a review of medical history, visual acuity tests, and measurement of intraocular pressure. Eye doctors use various instruments to assess the overall health of the eye and the optic nerve status.
During the examination, dilation drops might be applied to widen the pupil, allowing for a better view of the optic nerve and potential signs of damage. This dilation process may cause temporary sensitivity to light and blurred vision, but it is crucial for a thorough assessment. Additionally, the eye care professional may utilize a slit lamp, a specialized microscope that illuminates the eye, to examine the front and back structures in detail, ensuring no abnormalities are overlooked.
Visual Field Test
The visual field test helps determine if there are any blind spots in the peripheral vision, which can be indicative of glaucoma. Patients may be asked to look straight ahead and recognize lights or objects as they appear in their peripheral vision, providing a comprehensive view of their visual field. This test is vital, as early detection of peripheral vision loss can lead to timely intervention and management of the disease.
Moreover, the visual field test can be performed using various methods, including automated perimetry, which utilizes a computer to map the visual field, and confrontational testing, which is a more basic method often used in initial screenings. The results from these tests can help eye care professionals track the progression of glaucoma over time, allowing for adjustments in treatment plans as necessary. To read more about how visual field test are done click here.
Optical Coherence Tomography
Optical coherence tomography (OCT) is a non-invasive imaging test that provides detailed cross-sectional views of the retina and optic nerve. This advanced technology can detect subtle changes in the nerve fiber layer thickness, assisting in the early diagnosis of glaucoma. The OCT scan is quick and painless, making it a preferred choice for many patients.
In addition to its diagnostic capabilities, OCT can also be instrumental in monitoring the effectiveness of treatment over time. By comparing OCT images taken at different intervals, eye care professionals can assess whether the disease is progressing or stabilizing, guiding decisions on medication adjustments or surgical interventions. This level of precision in monitoring is invaluable, as it allows for a more personalized approach to managing glaucoma, ultimately aiming to preserve the patient’s vision for as long as possible.
Treatment Options for Glaucoma
Treatment for glaucoma focuses on lowering intraocular pressure to prevent further optic nerve damage. The choice of treatment may vary depending on the type and severity of glaucoma.
Medication and Eye Drops
Medications are often the first line of defense against glaucoma. Prescription eye drops can reduce intraocular pressure by decreasing fluid production or improving drainage. Common medications include prostaglandin analogs, beta-blockers, and alpha agonists.
Consistency in using medications is vital. Patients should follow their doctor’s instructions carefully and report any side effects, as many medications may have adverse reactions. Additionally, it is important for patients to schedule regular follow-up appointments to monitor their intraocular pressure and assess the effectiveness of the prescribed treatment. This ongoing communication with healthcare providers can help in making timely adjustments to therapy, ensuring optimal management of the condition.
Laser Treatment
For patients who do not respond adequately to medications, laser treatments can provide a viable option. The two primary types of laser procedures are laser trabeculoplasty and laser iridotomy.
Laser Trabeculoplasty: This procedure enhances fluid drainage by applying laser energy to the trabecular meshwork, helping to lower intraocular pressure. Patients often experience a quick recovery, with many returning to their normal activities shortly after the procedure.
Laser Iridotomy: Often used for angle-closure glaucoma, this involves creating a small hole in the peripheral iris to improve fluid outflow. This procedure can be particularly effective in preventing acute glaucoma attacks, which can lead to significant vision loss if not treated promptly.
Surgical Procedures
In more advanced cases, surgery may be necessary. Surgical options such as trabeculectomy or the implantation of drainage devices can effectively lower intraocular pressure.

During a trabeculectomy, a new channel is created for fluid to drain out of the eye, alleviating pressure. Drainage implants are also designed to provide continuous drainage of intraocular fluid, particularly in patients with severe glaucoma. These surgical interventions are typically reserved for cases where other treatments have failed, and they require careful consideration of potential risks and benefits. Post-operative care is crucial, as patients must adhere to follow-up appointments to ensure proper healing and monitor for any complications that may arise during recovery.
Furthermore, advancements in surgical techniques and technology have led to the development of minimally invasive glaucoma surgeries (MIGS), which offer promising alternatives with shorter recovery times and fewer complications. These innovative procedures aim to reduce intraocular pressure while preserving the eye’s natural anatomy, making them an appealing option for many patients. As research continues to evolve in the field of glaucoma treatment, patients are encouraged to discuss all available options with their eye care specialists to determine the most suitable approach for their individual needs.
Living with Glaucoma
Managing life with glaucoma can be challenging, but there are ways to adapt and maintain a good quality of life. Education about the disease and its management is essential for empowering patients and their families.
Lifestyle Adjustments
Incorporating certain lifestyle changes can support eye health and overall well-being. Regular exercise can be beneficial for maintaining healthy eye pressure, while a balanced diet rich in antioxidants may contribute to retinal health.
Regular check-ups with an eye care professional
Avoiding smoking, as it can worsen the risk of vision loss
Managing stress through relaxation techniques
Coping Mechanisms and Support
Many individuals may feel overwhelmed or anxious upon receiving a glaucoma diagnosis. Seeking support from friends, family, or support groups can aid in coping with emotional challenges.
Additionally, utilizing resources such as counseling, educational workshops, and advocacy organizations can provide valuable information and support to those living with glaucoma.
In summary, understanding the symptoms, diagnostic procedures, and treatment options for glaucoma is crucial for effective management. By staying informed and proactive, individuals can safeguard their vision and maintain a good quality of life.